5 yo F with no significant medical history presents for 4 days of URI symptoms, cough and fevers Tmax 102. Parents report she is not getting better. States cough is dry but "harsh". Has been getting some intermittent hives but responding to loratadine. Parents report a decrease in po intake but no vomiting or diarrhea. No abdominal pain. Family denies any increase in work of breathing.
VS T 101.2F HR 125 BP 90/50 RR 26 O2 96% on RA
Physical exam
Gen: well appearing no retractions or tachypnea good color + dry cough
HEENT: Wnl
CVS: tachycardic
Lungs decreased breath sounds to left middle lobe no wheezing no crackles
Abd soft ndnt exam
Skin warm well perfused good cap refill
Do you x-ray? Or reassurance and discharge???
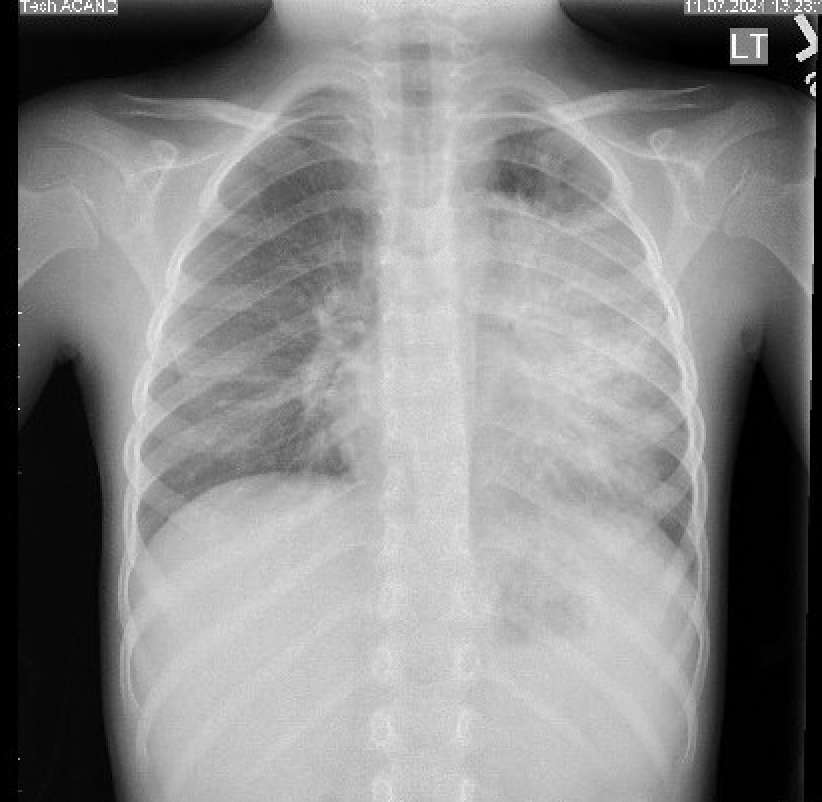
Chest- xray! (You would expect patient to be improving at this point and not getting worse + pulse ox of 96% on RA which should prompt you to pursue imaging).
What would your antibiotic choice be?
Can she be discharged or does she require inpatient admission?
MYCOPLASMA PNEUMONIA
Community acquired pneumonia is frequently seen in the ED. The first line antibiotic choice has been amoxicillin 90 mg/kg/day (BID) but, over the last few months ,we have seen a rise in Mycoplasma pneumonia infections. After a decrease in respiratory infections due to COVID-19 restrictions, M. pneumoniae is re-emerging and now appears more frequently in pediatric emergency visits. The increase has been particularly notable in children aged 2–4, a group not traditionally considered high-risk for M. pneumoniae pneumonia. Recent surveillance by the CDC indicates that as of fall 2024, the positivity rate for Mycoplasma pneumoniae in respiratory panels has climbed, reflecting a seasonal peak in August.
This resurgence underscores the importance of recognizing M. pneumoniae in pediatric cases of community-acquired pneumonia, especially when symptoms persist despite beta-lactam antibiotics, which are ineffective against this organism. Most cases respond to macrolide antibiotics, such as azithromycin, which remain the first-line treatment despite the rare presence of macrolide-resistant strains in the U.S.
Typically, Mycoplasma infections cause a more diffuse or patchy interstitial pattern on chest X-ray, rather than the consolidated appearance seen in classic lobar pneumonia caused by bacteria like Streptococcus pneumoniae.
However, in some cases, Mycoplasma can mimic lobar pneumonia, especially in children and young adults, where an entire lobe may appear consolidated on imaging. This occurs due to localized inflammatory responses in the lung, though it's often still less dense than the consolidation associated with typical bacterial lobar pneumonia.
Testing for mycoplasma can be done with a nasopharyngeal or oropharynx swab. Mycoplasma PCR can also be tested in the blood but does not return during an ED visit. Shared decision making with parents can be done to either prophylactically start treatment or give close return precautions if no improvement in beta lactam coverage. The first line treatment for mycoplasma is azithromycin for 5 days. Start at 10mg/kg on day 1 then subsequent days (2-5) 5mg/day. For patients with allergies or intolerance, doxycycline can be given for age 8 and above.
Decisions for inpatient admission are the same as those for community acquired pneumonia
Respiratory distress and/or hypoxia
Inability to tolerate PO.
Chronic medical conditions that may complicate the course of treatment.
Extrapulmonary complications
Mycoplasma pneumoniae Induced Rash and Mucositis (MIRM): Treat with macrolide. Will also require wound care/burn management if severe enough. Not all rash including mucosal surfaces is EM/SJS/TEN. Consider mycoplasma infection.
https://pedemmorsels.com/mycoplasma-pneumoniae-induced-rash-and-mucositis/
Mycoplasma Pneumoniae Induced Rash and Mucositis — Pediatric EM Morsels
Mycoplasma Pneumoniae Induced Rash and Mucositis (MIRM) may look like Stevens Johnsons Syndrome, but it is not. Let's Review.
pedemmorsels.com
TAMA'S TIPS
HIGHLY CONSIDER ADDING AZITHROMYCIN TO YOUR CURRENT CASES OF CAP
See some references below for recent CDC communication regarding the current state of affairs.
https://www.cdc.gov/ncird/whats-new/mycoplasma-pneumoniae-infections-have-been-increasing.html
Mycoplasma Pneumoniae Infections Have Been Increasing
Bacterial infection increase is especially affecting young children, causing pneumonia.
www.cdc.gov
https://www.cdc.gov/mmwr/volumes/73/wr/mm7307a3.htm
Notes from the Field: Reemergence of Mycoplasma ...
This report describes an increase in Mycoplasma pneumoniae, a common cause of respiratory illness, beginning in fall 2023.
www.cdc.gov

