THIS IS CONTENT NOT USED FROM THE OLD SITE
Side links
Congrats to the @SIUHOSPITAL house staff chairs Dr. Mustafa and our very own Dr. Catherine Park @elie_charabaty… https://t.co/8Ayhdo6M53
RT @abbashu: #embound #match2022 Don’t miss this podcast from @ALiEMteam Sage advice and reflections from PDs including… https://t.co/yxdB9OdkNx
Happy Medical New Year to our interns - halfway done with orientation already! @SIUHOSPITAL @Billycaps_MD… https://t.co/oqwJf7PvQQ
RT @abbashu: Had a great time celebrating @statenislandem #Classof2021 last night. These future leaders will not disappoint… https://t.co/Uui3StefEJ
RT @ercowboy: Chief Resident's Day in Central Park with #ALLNYCEM! @treatNstreetEM @jbeckesmay @abbashu @lmelville535… https://t.co/MaNIUaqtv3
RT @abbashu: Brilliant innovation by Dr. Kong @statenislandem for #PedsICU #foamcc Airway equipment organization in our recusss… https://t.co/M14aKxQ7ic
RT @abbashu: Joint venture with @StatenIslandRad and @statenislandem in a new blog #RadsRounds #MedTwitter @SIUHOSPITAL Case 1… https://t.co/F7Hb7RUi2N
RT @MSingh_MD: @statenislandem up as the third team in the finals...anxiously awaiting the decision from judges @ersimulationdoc,… https://t.co/BQpMEM3cDI
RT @MSingh_MD: Excited for the 2021 #ALLNYCEM Virtual SIMWars Finale at 3pm today! @StJohnsEMRes @statenislandem @Northwell_EM https://t.co/tkWbJCZQhJ
Crash Course in Emergency Ultrasound
A free course designed by Dr. Josh Greenstein, an Ultrasound Fellowship-trained EM attending at SIUH, offered to medical students interested in an EM residency. Contact Dr. Josh Greenstein (joshgreenstein@gmail.com) for any questions.
July 22 and August 19 only! 8:30 AM - 4 PM
8:30 - 9:00 AM: Welcome
9:00 - 9:30 AM: Learning how to use the Ultrasound machine
9:30 - 10:15 AM: Extended FAST examination
10:15 - 10:30 AM: Break
10:30 - 11:00 AM: Ultrasound-guided central lines
11:00 - 11:30 AM: Cardiac Ultrasound examination
11:30 - 11:45 AM: Break
11:45 - 12:15 PM: Flank Pain assessment with Ultrasound
12:15 - 12:30 PM: Soft Tissue Ultrasound
12:30 - 1:30 PM: Lunch
1:30 - 4:00 PM: Hands-on session (1-on-1 training on live models; central line practice on Manikins)
Space is limited - sign up below!
Life in NYC
Staten Island University Hospital is located in Staten Island, a borough of New York City, just 20 minutes from midtown Manhattan. The location is ideal for its close proximity to Manhattan and ability to enjoy suburban life. Our faculty and residents live in Brooklyn, Manhattan, New Jersey, and Staten Island.
New York is a great place to spend the three years of your residency. It boasts great nightlife, music, theatre, and restaurants. For sports fans, you can’t help but become an enthusiast of at least one of the New York teams. With 2 major league baseball teams, 2 NFL football teams, an NBA basketball team, and 2 NHL hockey teams, there is something for everyone. You can easily spend your day in the city rollerblading in Central Park, visiting the Guggenheim or the Metropolitan Museum of Art, shopping in SoHo, or just relaxing in the Village.
Staten Island is the perfect getaway from the busy hustle and bustle of urban activity. The Island has miles of coastline on both its North and South shores, with superb swimming, sailing, boating, water skiing, and fishing. There are many fine restaurants and shopping is plentiful.
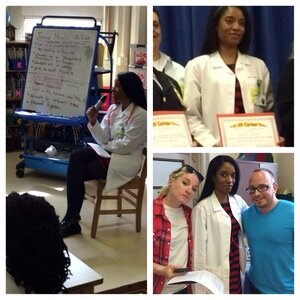
Our mission is to provide youth mentorship with a focus on higher education of minority students, as we are historically underrepresented in the medical community and to educate the community on health related issues. Contact Afoma Ndubuisi to get involved in mentorship and upcoming events.
Upcoming Events
Career day and classroom visits- TBA
Nursing home visits- TBA
Past Events
Food Pantry Volunteering at the Council of Jewish Organizations of Staten Island (January 21, 2015)
Served, fed, and distributed pantry bags to families in need.
Boys Will Ascend educational forum (October 18, 2014)
A program that targeted pre-teen and teenage young men to steer them from bad choices and toward a goal-oriented, purposeful future.
Amplify your Voice by Island Voice's Mentor/Mentee program (August 26, 2014)
Supported Staten Island youth with diverse background in self expression through art, spoken word, and music.











Wellness Getting Started
It definitely was mine. And probably a large proportion of my colleagues.
See I'm the daughter of a tough Greek man. Spartan actually. And I also happen to be a young Emergency Medicine attending. People like me, and most of you out there reading this are taught to suck-it-up and push through things. How else would we have made it through medical school, the multiple USMLE tests, Emergency Medicine "audition rotations", "THE MATCH", and finally residency?
But the problem with this "Superman" mentality is that it's not sustainable. Not for the average physician who plans on living a happy life inside and outside of medicine.
I used to think that if I can just make it through medical school and get into residency I will be fine. And then I got into the exact residency that I wanted and I thought "okay, if I can just get through residency then I will be happy and life will be okay".
This thinking is clearly flawed. Because once residency come and goes after three to four grueling years of literally blood, sweat and tears you graduate. And then your career actually begins.
Learning about wellness and discussing topics such as physician burnout, sleep management, financial planning, and breathing exercises might seem like secondary to learning about Neonatal Resuscitation, the different doses and uses for TPA and sepsis vs SOFA but actually it might be more important.
Yup, I said it. More important. Because what's the point of learning all this medical literature if we burn out, switch careers, hate going into work every day or even tragedly commit suicide?
Seems dramatic, but its true. And for those of you out there who are still skeptical I hope that our Wellness and Resilience Program at SIUH will help soften you, and in the process paradoxically make you a stronger, and more resilient physician.
Wait, WHAT? Hold on a second.
What in the world is this "resilience" thing??
"THE ABILITY TO BOUNCE BACK IN THE FACE OF A STRESSOR OR CHRONIC STRESS; THE ABILITY TO THRIVE IN THE FACE OF HARDSHIP AND CHANGE"
English please?
In order to succeed as emergency physicians and live a long and happy career, we have to learn concepts and practice exercises that will make stress and problems roll off our shoulders instead of annoy us or frustrate us. It's not always easy to do in the fast-paced high-stress nature of our jobs. But it's possible.
Picture this. You are working a 7a-7p Sunday shift in the main ER. It's 1pm and know you're realizing you just picked up one too many patients. The troponin on your 66 year old diabetic diaphoretic man with chest pain has been processing for over 2 hours. The medicine resident refuses to take your admission until the urinalysis is back on your elderly lady who clearly has a simple pneumonia and is already getting appropriate antibiotics anyway. Your electronic documenting system keeps freezing and now you have to restart your computer for the third time. All while you keep getting phone calls from your consultants who are asking one million questions and that annoying family member is standing over you asking "is the CT report back yet? We've been here forever" after the patient literally just returned from the CT scanner.
How do you respond? How do you react? What is going through your mind? For most people they don't just roll their eyes, laugh and finish the shift gracefully.
Resiliency is a relatively new concept in our field. But it's real and it's a skill that can be taught and we hope to teach you through our Wellness and Resilience Program.
I hope you enjoyed this introduction to our Wellness and Resilience Program at SIUH. We will be giving lectures at our conferences throughout the year, posting and distributing blog-style articles written by colleagues and most importantly having open discussions about these emergency medicine topics.
Stay tuned. More to come!
Frosso Adamakos, MD
Emergency Medicine Attending Physician
SIUH Wellness and Resiliency Curriculum Director
Sleep Management
A pretty common reason you or many of your colleagues joined the field. Besides it being the greatest specialty of course. However, the flexibility shift work affords comes at a price.
A 2008 ABEM study found that 43% of EM physicians contemplated leaving EM due to night shifts and 51% reported negative health and well being effects. An ACEP statement maintains that the adverse effect of constantly rotating shifts is the single most important reason given for premature attrition in the field.
Whoa.
Shift work has been linked to hypertension, lower fertility, GI ulcers, metabolic syndrome, type 2 diabetes, decreased immune system and higher rates of cardiovascular mortality and car accidents.
As if that’s not enough compared to the normal “9-5 worker”, shift workers chronically exhibit higher rate of irritability, exhaustion, depression, aggressive behavior, and poorer levels of performance, incoordination, and impaired complex task learning.
Basically shift work wreaks havoc on our bodies.
An emergency physician by the name of Paul Austin highlighted very well what most of us feel walking into a night shift in his book ‘Something for the Pain’. “I’ve been an attending physician for ten years and nights are still scary. No one works as efficiently at night as they do during the day. The Exxon Valdez oil spill, the Three Mile Island meltdown, and the Bhopal Plant Explosion all happened on the night shift. I just want to make it to daylight without hurting someone.”
So shift work is bad for us, but it’s not going away. In fact many traditional daytime functions are now expected 24/7. Even more reason for this discussion. Below are some strategies to maximize good quality sleep and minimize the harmful effects of shift work.
DAILY HABITS
-When shifting from nights back to days go to sleep as soon as possible after your last shift ends and get up after 4 hours. This will restore you enough to salvage the day, while leaving you tired enough to sleep that night. Sleeping more than 4 hours will retard the sleep cycle that night, causing loss of REM sleep.
-Avoid naps unless absolutely necessary. Naps are best during natural metabolic troughs (2-3PM and 2-4AM). Don’t nap more than 1 hour, it can cause sleep inertia (that groggy feeling you get after sleeping too long).
-Be selfish with your sleep. Take time for family, friends and hobbies before your shift, but let those around you know your schedule and how important it is to sleep.
-When transitioning from days to nights try to keep up with “anchor sleep”. Anchor sleep is a few hours almost every night that your body is asleep. For instance if you sleep 10-6 during the week and 1-9 on the weekend, 1-5 is your anchor sleep, and your body can always rely on sleep between 1 and 5. Your body craves for that consistency. Everyone has a different transitioning method but by sleeping close to your normal times the night before, having minimal caffeine in the morning, then taking a nap in a cool, quiet, blacked out room your body has a better chance of naturally transitioning.
FOOD AND DRUGS
- Avoid caffeine within 6-8 hours of bedtime
-Low doses of non-habit forming sleep aids such as melatonin and Benadryl are a safe alternative sleep aid. Melatonin is thought to help reset circadian rhythms
-Alcohol and fatty foods cause fragmented sleep (more time in stage 2 sleep), avoid them when working nights.
FALLING ASLEEP
-Avoid computer, phone and TV screens before bed. The light spectrum they emit can suppress melatonin.
-Get blackout curtains and keep your room between 60 and 70F. Dark and cool is ideal for sleep.
-Purchase white noise machines, or phone apps to block background noise. Even noise that doesn’t wake you can be enough to shift you from deep sleep (REM) to shallow sleep (Stage 1-2) and cause sleep fragmentation.
WAKING UP
- Bright lights will help you wake up, when you get out of bed turn on all the lights and open the blinds.
-Exercise keeps you awake. Workout after waking, not before bed. Studies have shown exercise helps to speed circadian shifts.
AFTER THE SHIFT
-Wear sunglasses when you leave the hospital in the morning and have your apartment cool and dark for your arrival. Even brief exposure to sunlight will suppress melatonin and disrupt your circadian rhythm
At the end of the day there is no perfect way to transition your body back and forth from days to nights. Shift work is hard but we can do things to try to make it easier. One of the most important things you can do is educate your family and friends. Apologize to them in advance for your upcoming crankiness during your string of nights and ask for their help during this time. We hope that this information will help you find something that works for you.
DR. LAWRENCE O'HALLORAN
SIUH EM RESIDENT
Resources:
http://www.medscape.com/viewarticle/830928
http://www.augusta.edu/mcg/clerkships/em/documents/shiftwork.pdf
https://akosmed.com/2015/12/30/dragging-struggles-with-shift-work-and-circadian-rhythms/
https://www.acep.org/clinical---practice-management/emergency-physician-shift-work/
https://www.acep.org/content.aspx?id=22728
http://www.acepnow.com/article/combat-sleep-disorders-from-working-night-shifts/2/
Resiliency
I would like to challenge the notion that physicians, especially us emergency physicians, are supposed to BE TOUGH and POWER THROUGH at all times.
HOW ABOUT INSTEAD WE SHIFT OVER TO THINKING OF OURSELVES AS THE CALM AND FOCUSED LEADER WHO IS CONSTANTLY SURROUNDED BY CHAOS.
THIS notion is the definition of resilience. The resilient physician is one who thrives in a state of constant stress, change and hardship. That doesn’t mean just trudging through and doing the job at hand. It means knowing how to bend and move with our stressors, not against them.
So… How do we learn to become this force field that allows stress to bounce off us and not bring us down?
MINDFULNESS
Below are some basic meditation tips to help you refocus your thoughts and go back to feeling calm when you’re feeling overwhelmed and like you’re about to break at work. We have all been there. It’s not a sign of weakness it’s just a fact with our jobs.
PRACTICE THESE AT REST at home for a few seconds every few days. You can’t expect an intern who’s never intubated a live person to successfully intubate the crashing variceal bleeder the same way you can’t expect to magically relax while the ER is going crazy and about to implode.
- Take a few breaths. Breathe slowly and focus only on your breath. Feel the cool air going in through your nose and the warm air coming out through your mouth. After a few breaths notice the way your body and mind suddenly feel a little more relaxed. Practice this and will be handy in the resus bays. This simple technique is taught and practiced rigorously amongst our own US military.
- Stand, sit or lie down. For 10 seconds squeeze every muscle in your body and hold in your breath. Squeeze your forehead, your face, your shoulders, arms, abs, butt, legs and toes. After 10 seconds release. Notice the way your muscles feel relaxing and you can feel your blood flowing through them. That’s the feeling of full relaxation. With practice, you will be able to take a deep breath in, and breathe out and achieve relaxation on the spot when needed. This one is a common technique that originated in cognitive behavior therapy.
- A popular saying amongst resuscitationists and taught to me by mentors in residency… Before checking the patient’s pulse check your own. Find your heart racing? Stop, take one breath, then go on to your task at hand. Remember the anxiety/performance bell curve? A little anxiety is good.. it helps us stay sharp during the chaos… But too much is detrimental and decreases our performance drastically.
- And lastly and all time goodie. One you probably heard your mother tell you time and time again. Remember that most things in life can wait a few seconds for a response. Think before you speak and think before you act. Most people don’t have to be intubated at that very moment and most consultants don’t need an immediate response from you.
ACEP created The “Emergency Medicine Wellness Week” in 2016 with a goal to remind us to take care of ourselves, and not just others. Hopefully the Wellness and Resiliency Curriculum at SIUH has helped introduce some ideas and topics over the year to help you do just that. Visit their website if interested for further discussion and articles https://www.acep.org/emwellnessweek/
Frosso Adamakos, MD
Emergency Medicine Attending Physician
SIUH Wellness and Resiliency Curriculum Director
References
ACEP; “The Resilient Emergency Physician Manuscript”
Building physician resilience; P. Jensen P, K. Trollope-Kumar, H. Waters, J. Everson; Can Fam Physician 2008;54:722-9
Physician Resilience: What It Means, Why It Matters, and How to Promote It”; R. Epstein, M. Krasner; Academic Medicine, Vol. 88, No. 3 / March 2013
ACEP Wellness Week
USA Military Resiliency Training
Cognitive Behavior Therapy Basic Techniques
Burnout
A little post on BURNOUT
Again? Why are we talking about this…
For the continued skeptics, I’m going to try to convince you this is an important topic in EM and should be discussed, the same way the heart score and cardiac observation units should be discussed.
TO START= Year after year emergency medicine trained EM physicians are among the top 3 groups of physicians that burnout. Critical care, surgery and internal medicine are the other usual contenders.
A recent poll suggests that at any given point in time, 50% of EM physicians report currently being burned out.
Physicians who report signs and symptoms of burnout…
have extremely high rates of premature attrition from the field
provide poorer quality of care
have higher rates of error
higher rates of substance abuse, depression, anxiety and physician suicide
And finally, recent statistics show that on average * 1-2 physicians per day commit suicide in the USA*. Do I have your attention now?
***RECOGNITION: When is it more than just normal stress and it’s actually burnout?***
PHYSICAL AND EMOTIONAL EXHAUSTION
YOU ARE EMOTIONALLY DRAINED, DEPLETED AND WORN OUT BY WORK AND NOT ABLE TO RECOVER IN YOUR NON-WORKING HOURS
DEPERSONALIZATION
THE DEVELOPMENT OF A CONSTANT NEGATIVE, CALLOUS AND CYNICAL ATTITUDE TOWARD PATIENTS AND THEIR CONCERNS
REDUCED SENSE OF PERSONAL ACCOMPLISHMENT
THE TENDENCY TO SEE YOUR WORK NEGATIVELY, WITHOUT VALUE OR MEANINGLESS (“WHAT’S THE USE?”) AND SEE OURSELVES AS INCOMPETENT (“THERE’S NO POINT”).
Keep in mind that nothing in life is black or white. A physician is not constantly resilient or constantly burnt out. Rather we can easily move from one end of this spectrum to the other.
***PREVENTION AND RECOVERY***
So now that we know what burnout it, before we start feeling toasty what can we do to prevent it? Or what if you are already starting to feel it? It’s okay! The same tips below are useful for prevention and recover from burnout.
BE MINDFUL
CHECK IN ON YOURSELF THROUGHOUT THE SHIFT AND RECOGNIZE WHEN YOU ARE STARTING TO TENSE UP. RECOGNIZE WHEN YOU ARE FEELING LIKE WORK IS TAKING OVER YOUR LIFE AND THERE IS NO WORK-LIFE BALANCE.
LEARN WHAT YOUR PERSONAL LIMITATIONS ARE AND CREATE A PLAN TO IMPROVE
DON’T FIGHT STRESS, JUST NOTICE IT THEN RELEASE IT
IT’S PHYSICS! WHEN YOU TRY TO FIGHT SOMETHING, IT WILL FIGHT BACK EVEN HARDER. WHEN STRESS OCCURS, NOTICE THE NEGATIVE EMOTIONS THAT COME WITH IT, THEN LET IT GO.
KNOW WHAT YOUR PROFESSIONAL DEMANDS ENTAIL AND BUILD ACCEPTANCE OF THEM… THEY AREN’T CHANGING AFTER ALL. AS WE DISCUSSED BEFORE WORK WITH YOUR STRESSORS NOT AGAINST THEM.
SEARCH FOR YOUR SENSE OF COMPASSION AND EXERCISE IT
REMEMBER THAT LITTLE PRE-MED STUDENT? WHY DID THEY WANT TO BE A DOCTOR?
PUT YOURSELF IN YOUR PATIENT’S SHOES… LIKE REALLY DO IT. A DIFFERENT PERSPECTIVE CHANGES EVERYTHING
RESTORE BALANCE IN YOUR LIFE
PRACTICE LIMIT SETTING… SAY NO!
YOU DON’T HAVE TO TAKE ON EVERY PROJECT THAT COMES YOUR WAY OR EVERY OUTING. DELEGATE PERSONAL AND PROFESSIONAL WHERE YOU CAN. SAY NO TO PEOPLE AND LEARN HOW TO TAKE THINGS OFF YOUR PLATE SO YOU’RE NOT CONSTANTLY OVERWHELMED.
UTILIZE PEER SUPPORT AND REACH OUT TO YOUR PERSONAL SUPPORT
THE MORE WE BUILD A CULTURE OF OPENNESS AND SUPPORT IN OUR COMMUNITY THE BETTER WE WILL BE PREPARED FOR THE STRUGGLES THAT COME OUR WAY. TALK ABOUT THAT REALLY SAD CASE WITH A COLLEAGUE AND THEY WILL PROBABLY HAVE A SIMILAR STORY THAT WILL HELP YOU REALIZE IT’S NORMAL TO FEEL THE WAY YOU DO AND THINGS WILL GET BETTER. I’M NOT TALKING ABOUT A SOB FEST HERE… EVEN JUST A FEW MINUTES BETWEEN SHIFTS OF CHIT CHAT CAN HELP EASE UP YOUR TENSION.
AND MOST IMPORTANTLY, ALWAYS PUT YOURSELF FIRST. PERIOD.
IT’S LIKE WE TELL OUR PATIENTS. IF YOU DON’T TAKE CARE OF YOURSELF HOW WILL YOU BE ABLE TO HELP OTHERS? MAKE YOURSELF A PRIORITY.
ACEP created The “Emergency Medicine Wellness Week” in 2016 with a goal to remind us to take care of ourselves, and not just others. Hopefully the Wellness and Resiliency Curriculum at SIUH has helped introduce some ideas and topics over the year to help you do just that. Visit their website if interested for further discussion and articles
Frosso Adamakos, MD
Emergency Medicine Attending Physician
SIUH Wellness and Resiliency Curriculum Director
References
The Happy MD; “Physician Burnout, Why it’s Not a Fair Fight”
ACEP; “The Resilient Emergency Physician Manuscript”
December 2016 EMRAP LIN Session Resident Wellness
Physician Resilience: What It Means, Why It Matters, and How to Promote It”; R. Epstein, M. Krasner; Academic Medicine, Vol. 88, No. 3 / March 2013
AMA; “How to beat burnout: 7 signs physicians should know”
Additional Forms
Case Writer template: Fill in the blank areas and e-mail your case for submission.

